“The problem with this disease is it’s a journey.”
— Cyndi Lauper on psoriasis
In 1936, New York dermatologist Paul Bechet summed up the frustration of psoriasis in the first sentence of an article for the Journal of the American Medical Association.
“Psoriasis is an antidote for dermatologists' ego,” he wrote.
“It is the most vulnerable point in their armour as experts, and it remains the most baffling of dermatoses despite the great advances recently made in dermatology.”
References to the painful skin condition go as far back as Hippocrates in 400 BC, who used coal tar and topical arsenic to treat it.
A lot has changed since then.
Today, an increasingly broad line of biologics is being developed that can often completely clear up the nagging problem.
You’ve heard or seen the commercials for Otezla, Humira, Skyrizi and other drugs. Bouncy, upbeat music accompanies carefree people twirling around at beaches and barbecues with their arms in the air, shoulders and bellies bare.
That wasn’t the case for Deva Murthy when she was first diagnosed with the condition in the 1980s.
From the age of 11 on, Murthy underwent tedious bouts of coal-tar baths, ultraviolet light therapy and even slathering her skin in ointments and enveloping herself in Saran wrap.
“As you can imagine, it’s very dehumanizing,” the Long Harbour resident said in an interview Thursday. “As an adolescent, it was particularly difficult.”
In elementary school she spent an entire year in hospital, the skin condition was so bad.
Eventually she was prescribed immunosuppressants like methotrexate and cyclosporine to control the autoimmune condition, despite the risk of harsh side effects and organ damage.
“It was a tough decision, but I was desperate. My whole body was covered, so I took whatever they offered me.”
That was before biologics came along about 15 years ago. Since then, she’s been virtually rash-free, except for an outbreak last year when she got too much sun on a trip down south. A newer line of drug cleared that up.
“I can’t say enough,” she said “These are life-changing medications.”

From ‘if’ to ‘when’
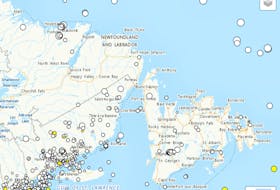
Psoriasis, which causes red, crusty patches of skin covered with scales, is more common in Newfoundland and Labrador than the rest of Canada. It can cause pain, including joint involvement, and can be an agonizing source of social stigma.
Many people mistakenly believe it’s contagious. It’s not.
St. John’s dermatologist Dr. Wayne Gulliver has witnessed the changes in treatment over 30 years, and the impact they’ve had on patients.
“Before it was, ‘if we get you better.’ Now it’s, ‘when are we going to get you better.’”
Usually within six months to a year, he says, patients end up between 75 and 100 per cent clear.
“The response is usually, ‘Doctor, you’ve given me back my life,’” he says.
“Before, everything was around their psoriasis. What they wore, when they went out.”
The drugs are much better targeted and safer than the suppressants he used to prescribe.
“If we look at the safety profile, we don’t see the severe infections or things that you see with other immune drugs.”
While he prefers patients ask their doctors for advice, Gulliver downplays the obligatory litany of risks cited on television advertisements.
“During the clinical trial, with 10,000 patients, if someone got an ingrown toenail, was it caused by the drug? Probably unlikely. Do they end up listing it? Yes.”
Those advertisements slip through on American channels, because Health Canada prohibits linking a specific drug to a condition in ads.

New and approved
In some ways, Murthy was lucky her condition was as bad as it was, because she received authorized use of the drugs for trials. They are otherwise extremely expensive.
This has been a problem for Newfoundland patients, but the tide is finally changing. Effective Sept. 20, the province listed one of the latest drugs, Skyrizi, in its formulary.
Murthy has been an executive with Psoriasis NL (psoriasisnl.com) for many years, and is proud of the work it does as the only support group in the province.
They were holding support-group meetings the third Wednesday of every month, but they’ve been on hold since the beginning of the COVID-19 pandemic.
She’s also grateful for Gulliver’s guidance as her specialist since she was a teenager.
“He was an immense emotional support for me and my family because it took a heavy toll back in those days,” she said.
Peter Jackson is a Local Journalism Initiative reporter covering health for The Telegram